On a balmy Easter Sunday in Palm Beach, Florida, 46-year-old realtor and COVID survivor Kristen Kearney got in her black Cadillac, drove 40 miles south to Pompano and boarded a OneBlood bus, a mobile blood and plasma donation facility where she’d spend the next few hours donating her convalescent plasma in the hopes it might save a life. (Recovered patients produce antibodies against coronavirus, and it’s thought that transfusing them into a sick patient might boost their immune response enough to fight it off.)
In just a few minutes, she was hooked up and ready to go. The machine whirred as it coaxed the blood from her veins, separating out the plasma before returning the rest of its components to her body. Soon, it would be passed off to a courier, tested for coronavirus antibodies at a separate lab and then whisked off to a nearby hospital where it would be transfused into a dying man she’d never met.
In the meantime, all she could do was wait. For 90 minutes, Kearney sat connected to the machine, chilly from the frigid air the phlebotomists pumped through the bus to keep donors from passing out. They gave her a Gatorade to stay hydrated, and three of them made small talk about the dark gold color of her plasma and the strange power of the device she was tethered to with see-through lines of ruby red.
To her surprise, it didn’t hurt a bit. In fact, as Kearney relaxed into the plushness of the reclined donation chair, the only thing she felt was relief. Four days earlier, she’d come across a Facebook post from a contact who was desperately seeking plasma for a 61-year-old man named Reno Boffice. An “upstanding” and beloved school principal in Lantana, Florida, who was known for his legendary sense of humor, love of animals and devotion to his students and family, Boffice had developed a severe case of COVID and had been transferred to the ICU. In the Facebook post, a friend of his wrote that he was “putting up a great fight” but needed plasma urgently.
Kearney didn’t know him, but something about him seemed kind. Having seen the ads for convalescent plasma donation on Facebook and the countless posts from other families seeking donors, she was already well-aware that as a survivor, her plasma might be able to help him. She contacted them right away and told them she wanted to donate. “I felt it was the right thing to do,” she says. “I thought my efforts would be small in return for the reward of trying to help save a life.”
Boffice’s family jumped at the opportunity. Almost immediately, they put her in touch with his doctor and welcomed her into their circle, grateful to have found a potential donor who was willing to give her plasma to a man she’d never met. Excited, she told them she still needed to be re-tested to confirm she was fully recovered, and that she’d update them on her progress.
“Progress,” however, was hard to make. Though she had every intention of doing what she could to save Boffice’s life, she had no idea that her earnest attempt to do so would become one of the more opaque and frustrating experiences of her own. After what she went through to get there — a frantic search for tests, apathetic nurses who turned her away and a maze of red tape so thick and winding she wondered if she’d ever be able to donate at all — the fact that she made it onto the Big Red Bus was its own Easter miracle.

As the coronavirus pandemic rages on into its fifth month, so does the race for both a treatment and a cure. Everything from anti-malaria drugs to black-market cat meds to bleach injections has been suggested and tried, and although there are more than 70 clinical trials of potential treatments currently registered with the FDA, none have been proven to work and many of them have put critically ill patients at even greater risk than the virus itself. Even remdesivir, an antiviral hyped up by the White House and pharmaceutical giant Gilead, has shown uncertain results — while a recent trial by the National Institutes of Health demonstrated that it can reduce recovery time in some patients, other studies have found that it’s no better at saving lives than a placebo.
In the meantime, millions of people are dying, symptoms are diversifying and the mood in the scientific community has grown desperate. As “Kate,” a pseudonymous trauma center nurse at a Southeastern U.S. hospital supervising nearly 250 positive or presumptive COVID patients tells us, doctors and researchers have grown indiscriminate in what they’re willing to try, throwing whatever’s safe at the wily and unpredictable virus as they search for “any port in the storm.”
As far as ports go, convalescent plasma therapy (CPT) — the process Kearney wanted to donate her plasma for — has been one of the more promising. A well-established procedure that involves removing antibody-rich blood plasma from a recovered patient and transfusing it into someone who’s still sick, CPT is thought to benefit patients by boosting their immune response enough to fight off the infection they’re suffering from. First used on a large scale during the Spanish Flu of 1918, it has since been used with some success to save the lives of patients suffering from diseases like polio, measles, H1N1, SARS and Ebola. Because a single donation can be transfused into three people and it poses little to no risk to the patients who receive it, it’s often referred to as “liquid gold,” an ace-in-the-hole that may succeed where other treatments fail.
But while CPT has always been a back-pocket option for physicians, the “chaotic” search for a COVID cure and the frenzied publicity surrounding it has started to pique the public’s interest in it as well. Just a few weeks ago, hardly anyone outside the medical community had even heard of convalescent plasma, but ever since the FDA greenlit CPT as an experimental therapy early last month, one thing has become overwhelmingly clear: Everyone and their mother suddenly wants plasma, and they want it now.
The thing is, few people are getting it. Though experts worry that it’s in critically short supply, an investigation into the country’s nascent COVID plasma efforts reveals that hospitals, blood banks and testing facilities across the country have been turning away qualified donors like Kearney, telling them their plasma isn’t needed and leaving them to fend for themselves amongst a confusing and contradictory system that appears to reject the very thing it’s built to collect.
And while these mistaken rejections are hardly the norm — tens of thousands of units of plasma have already been successfully collected and transfused — the fact that they’re happening at all raises an important question: Why are some donors being rejected, and could these mistakes be to blame for the country’s low stock of a potentially invaluable “last hope”?
But Is It Really Liquid Gold?
There are a million reasons why patients aren’t getting COVID plasma at the rate they should be, but any tension between the supply and demand for the so-called “liquid gold” can be boiled down to a single truth: No one knows if it actually works.
CPT has proven to be a decent approach for infections caused by other viruses, but so far, its efficacy as a treatment for SARS-CoV-2 — the virus that causes COVID — remains to be seen. While a few small studies and early reports from doctors treating the virus in China have shown promising results and a recent American study revealed the treatment is safe to use, plasma from recovered coronavirus survivors has not been shown to provide clinical benefits, and the FDA has yet to approve it as a viable treatment. In fact, the only reason it’s being used at all is because the FDA fast-tracked it as an Investigational New Drug (IND), meaning clinicians and researchers can use it in a limited capacity without having to subject it to randomized control trials to ensure its safety.
As such, COVID plasma comes with some pretty strict regulations, the most restrictive being who receives it. Right now, patients must be critically ill and hospitalized with what the FDA refers to as “severe or immediately life-threatening COVID-19 disease” in order to be transfused, but even then, it’s not a guarantee. The only way doctors can secure plasma for their dying patients is to make a special “expanded access” request, or enroll them in the large-scale clinical trial the FDA is overseeing.
It’s through the latter option that most patients get their COVID plasma. In April, the FDA kicked off a nationwide trial along with the Biomedical Advanced Research and Development Authority (BARDA) and the Mayo Clinic to study its potential as a treatment and, so far, most of the plasma collected by blood banks and hospitals has been collected and distributed with that goal in mind. But in order to examine whether COVID plasma is fact or fantasy — and get it to patients in need — the trial needs donors, and lots of them.
Thankfully, there’s been no shortage of willing COVID survivors like Kearney hoping to roll up their sleeves. As soon as the news broke that plasma was being studied and recovered patients could donate, hordes of them made appointments at collection facilities like the American Red Cross and OneBlood, and many more started social media campaigns and joined online donor groups to let patients in need know they were ready and willing to give.
Some were able to do so without a hitch and had the beautiful and gratifying experience of witnessing their recipients recover just days after being transfused. Kearney, however, did not. Her first roadblock was a testing glitch. In order to donate convalescent plasma for COVID, the FDA requires potential donors to show proof of a positive test for coronavirus and be symptom-free for anywhere from 14 to 28 days, depending on the facility collecting plasma. A negative test following their recovery or an antibody test that shows they’ve been exposed is also often required, but since Kearney had neither, Boffice’s doctor — whom she had begun to correspond with — recommended she visit a local ER to obtain her negative results.
But when she arrived, she — along with two other potential plasma donors — were turned away. A patient had already donated that day, a nurse told them. Besides, they were out of tests. They were reserved for the “sickest patients only,” and if any of them wanted one, the nurse said blithely, they’d have to be “admitted to the ER.” That struck Kearney as odd — with the amount of advertisements seeking COVID plasma she’d seen on social media, she’d thought there was a much greater need. Plus, weren’t the people dying in the ICU from coronavirus the actual “sickest patients”?
Kearney was thoroughly confused, but the experience only pushed her to keep trying. Holding the image of Boffice and his family in her mind, she promised herself she wouldn’t give up until her arm was hooked to a plasma machine. She set to work on a Plan B, unaware that her bizarre journey to the OneBlood bus had only just begun.
Meanwhile, for the thousands of other COVID patients in ICUs across the country, the great plasma experiment had already begun. At the same moment Kearney was plotting her next move, patients were being transfused with the precious, straw-colored liquid, and families and physicians alike perched breathless on the edge of their seats as they waited to see whether or not it would work.
Conclusive research on how COVID patients are faring after being transfused has yet to be published, but anecdotal reports from doctors, nurses and family members who spoke with us have been mixed. Provided their patients and loved ones were able to be transfused at all, plasma, like other experimental therapies, has been far from the miracle drug some have hoped it would be. While many patients have made astonishing recoveries after being transfused, others have died just the same.
This doesn’t surprise Joshua Le at all. A critical care physician in King County, Washington, who has been supervising severely ill COVID patients in the ICU since the start of the outbreak, he’s become hyper-aware of both the excitement — and the disappointment — that experimental treatments like hydroxychloroquine, remdesivir and now CPT can bring. “We shouldn’t forget that what we’re doing right now with plasma is experimental,” he says. “We’re really only doing this because we have no other option.” The frustration in his voice is obvious. “I spend all my time in the ICU treating patients who are dying,” he continues. “I just really hope this works.”
But though the evidence for CPT as a treatment for COVID is still limited, the demand for it is not. As limited data and encouraging news stories of full recoveries trickle in, doctors, blood banks and hospitals have begun to clamor for plasma in spite of its remedial uncertainty; they’ve issued pleas for recovered patients to donate, kicked off elaborate donation campaigns, released plans to build COVID plasma banks and attempted to raise an online infrastructure of websites where donors can sign up, get screened and start the process. Companies like OneBlood even started posting ads on Facebook, which is how Kearney says she found out about donation.
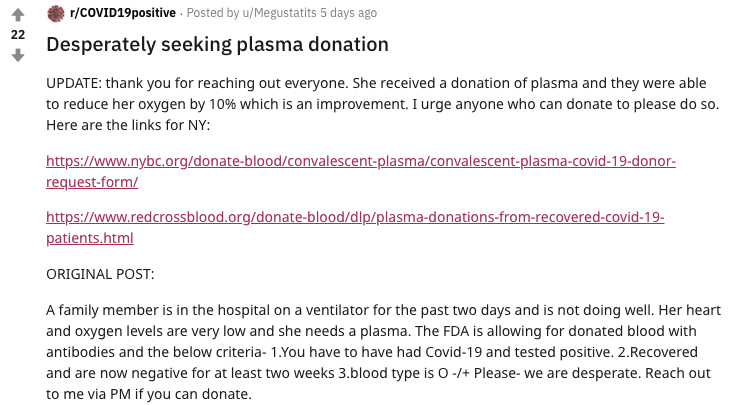
Meanwhile, families and friends of dying COVID patients post desperate pleas for donors on social media, surfing the endless scrolls for potential matches and begging their followers for help (though, it’s unclear whether they’re aware that directed donations aimed at specific recipients aren’t allowed in the Mayo Clinic study and no longer the norm outside of it).
“There is absolutely a shortage of plasma for critically ill COVID patients, both enrolled in the study and outside of it,” says Director of the Mayo Clinic Human Research Protection Program Scott Wright, explaining that only about two-thirds of the 16,500 patients in the Mayo Clinic trial have been transfused (it was only half when we originally interviewed him).
To be clear, that’s not normal, even for an investigational drug. As Wright explains, most drug trials are planned months to years in advance, and far more of the drug is made than what’s actually needed so that a shortage doesn’t affect the results. In the case of COVID, the situation has been so dire that the Mayo Clinic trial kicked off without much of a supply at all. And even though blood banks like the American Red Cross have their people working “around the clock” to secure COVID plasma from eligible donors, media relations manager Stephanie Rendon says its efforts are still being outpaced by the ever-growing number of critically ill patients whose lives hang in the balance between shortage and supply.
It would be helpful to throw out a figure for just how wide the gap between supply and demand actually is, but incredibly, the problem isn’t even quantifiable yet. As Nigel Paneth, an epidemiologist at Michigan State University and one of the organizers of the National COVID-19 Convalescent Plasma Project, explains, the number of patients in need of plasma is likely much greater than we know, and no good metric exists to take a tally. For one, not all critically ill patients are enrolled in the Mayo Clinic study (which means they’re not being counted), and two, no one’s even sure how many people have been hospitalized with the virus in the first place.
What’s more clear, however, is where that plasma is going. Most of the country’s recipients are on the harder-hit East Coast, where higher amounts of recovered patients correspond to a larger pool of qualified donors. In New York state, ICU nurse Cheryl Farrington says almost all of her intubated COVID patients have received plasma, but in Washington, Le says he was only able to secure two units from the Mayo Clinic study for a floor full of dying patients in April. Since then, he’s received an additional 15 to 20 units, but it’s still not enough — he says he needs twice that amount, and stat. “It isn’t easy to get on the West Coast,” he says. “I spent a lot of time calling local blood banks and trying to figure out where it all was and why we couldn’t get any.” In the meantime, he says, patients are dying.
Things at Memorial Health University Medical Center in Savannah, Georgia, are somewhere in between — three weeks ago, the hospital reported that it was only able to secure seven units of convalescent plasma to treat the roughly 30 critically ill COVID patients it had in the ICU. And while that’s certainly more than Le and other West Coast doctors have been able to get, it’s still not enough. As Todd Bruker, the hospital’s head of pathology and laboratory medicine, told Savannah Now, the demand is high, but the “supply just isn’t there yet.” Elsewhere, the story is much the same.
Drastically increasing plasma donations is the only fix, and as such, Le says donors are now being “treated like heroes.” And while accolades are far less important than altruism, successful donors have taken to the internet to issue rousing platitudes like, “It’s the least we can do,” and “Every donation counts,” with some even describing their donation experience as a “moral obligation” to help others. In triumphant Facebook and Instagram photos, they pose along imposing-looking plasma machines as blood is drained from their veins through long, see-through plastic tubes, only the faintest wince registering on their faces behind more obvious expressions of joy.
Kearney was familiar with these success stories, but her time to be a “hero” was still far off. The day after being rejected at the ER in Palm Beach, she tried again the next day with Boffice’s doctor, who, after hearing her experience at the hospital, made a valiant effort to find her a rapid test. But when she called to make an appointment to get it, she hit another wall: The test wouldn’t be rapid after all, and she’d have to wait five to seven days to obtain her results. Worse, she’d missed the laboratory pickup window.
By that point, she was “incensed” — how could a simple test be a roadblock to someone’s last hope? More importantly, why was it that other people were “doing the right thing” while she was getting sent down a rabbit hole?
Two days later, a close contact of Boffice’s, using his account to communicate with his friends and family, posted an ominous message on his Facebook page: “We have a donor; however, we cannot get the plasma to the hospital. There seems to be a disconnect in the process from the blood bank/donation site to the patient… Time is of the essence. This makes no sense, hope is just an arms’ length away and we can’t get hold of it.”
A thousand miles north in Baltimore, 35-year-old product marketer and new mom Kellie Burns was having a similar problem. Her father, a retired steamfitter who loved spending time with his six kids, was in critical condition on a ventilator in New York state. But though she’d found two donors whose blood type matched his, they couldn’t get re-tested, either. As a one-time technology consultant for hospitals with an understanding of the health-care industry, she expected the testing to be clunky, but after days of frenzied calls to blood banks, hospitals and health departments, trying to find tests and watching her father go from bad to worse, what started as a mere inconvenience turned into an all-consuming nightmare.
Some days, Burns was so busy trying to get plasma to her father that she didn’t even have time to get out of bed. From beneath her teal and white sheets, she’d make call after call as she frantically searched for donors and tests, barely stopping to consume the food her husband would lay on the nightstand in the hope that she’d let it rest for long enough to eat.
At times, her father’s nurses — dressed in protective “moon gear” — would video call her from his hospital bed, holding an iPad up to his face so she could talk to him. He looked peaceful and calm under his heavy sedation, unaware that far away, in her own bed, she was doing everything she could to save his life.
“When all you care about is your loved one and them surviving, you just want to get them the treatment that they need,” she says, recalling her experience. “It was just such a rollercoaster of emotions. Not only with my dad’s condition, but we also ran into so many dead ends with the donation process.”
Unbeknownst to both her and Kearney, they were far from alone.
How Things Are Going Wrong
This early on, it’s hard to tell exactly where the ball is being dropped, but a number of concerning trends in the plasma collection process have emerged over the past month that may explain the current chasm between supply and demand.
The first and most obvious is that there aren’t enough donors. Not for blood, not for regular plasma, not for any substance that can be sucked out of your veins at a blood bank, actually. Right now, as over a third of the world shelters in place, the fear of being in public — especially up close and personal with a phlebotomist who can’t exactly draw blood from six feet away — has caused thousands of would-be donors to cancel or postpone their appointments, leading to massive blood and plasma shortages experts worry could “lead to mortality” and “kill our patients.” Between March and May, OneBlood lost 50,000 potential donations after having to cancel 3,000 blood drives, and at the Red Cross, the story was much the same. So, it’s not just potential COVID plasma donors who aren’t showing up, it’s everybody.
Paradoxically though, showing up to a blood bank to donate convalescent plasma does not, in any way, mean you’ll walk out a donor. While Le says it’s tempting to imagine that any one of the country’s 281,000 recovered COVID survivors could stroll into the nearest blood bank and dole out their plasma, that’s not close to how the process works.
Besides being symptom-free for two to four weeks and showing proof of a positive test — which the vast majority of people with coronavirus were never able to get in the first place — potential donors must also test negative for HIV, Hepatitis C and a host of other infectious, blood-borne diseases that could put a recipient’s health at risk. Other unexpected traits may disqualify them, too. According to the Red Cross’ plasma donor eligibility requirements, potential donors cannot donate if they’re on certain acne medications, have leukemia, have gotten a tattoo in the past year in one of the 10 states that doesn’t regulate tattoo facilities, are a man who has had sex with another man in the past three months or have taken aspirin in the two days prior to donating.
These are the same requirements any blood or plasma donor must meet and are set up to protect the health of the patient receiving the transfusion, so while stringent, it’s critical that they’re reliably enforced.
Right now, it’s unclear how many potential COVID plasma donors are being disqualified by these requirements, but after speaking to a handful of local blood banks in King County about the shortage, Le estimates it’s anywhere between 80 to 90 percent (though that number is purely an anecdotal estimate). Rendon says only about 10 percent of donors qualify to donate COVID plasma at the Red Cross, but in other parts of the country, that number does appear to be larger.
If the roughly 10 to 20 percent of potential donors make it past that stage of the screening process, they must also prove that they’ve recovered from COVID with either a negative coronavirus test or a positive antibody test. For most donors, this is often the most difficult step: As Kearney and Burns experience, testing facilities are already reluctant to use precious supplies, let alone on recovered patients.
Kearney says she was only able to secure a secondary nasal swab because she spent days calling different hospitals and labs until she found one at a private lab in Miami. Because it was a holiday weekend, she had to take the specimen from the hospital to the lab herself, nestling it beside her in the passenger seat of her car like precious cargo while she sped down the deserted highway.
To be clear, that almost never happens. Francis Rodriguez, the registration supervisor at the testing facility at Larkin Community Hospital where Kearney got her second test, says protocol makes it “impossible” for a patient to transport their own specimen, and in Echo Park, California, a representative of Carbon Health, a primacy and urgent care facility offering coronavirus tests, says the only way something like that would happen is if the patient wanted to rush their order so badly that they couldn’t even wait for an expedited medical courier. Kearney, however, didn’t have the option of waiting — Boffice was dying, and she’d already been held up too long.
Meanwhile, an exhausted Burns had to badger the New York State Department of Health for days before they authorized a secondary nasal swab for a pair of potential donors hoping to gift plasma to her father. Eventually, a compassionate doctor at the Health Department was willing to hear her out and organize testing, but Burns says she would have never got them through the process if it weren’t for a few key people and an attitude of total, 24/7 perseverance. “We had to take complete control to make any of this happen,” she says. “I can’t imagine what it would be like for someone who had less access to this system than I did.”
And while the availability of tests has increased in some cities since she went through that process, hold-ups like that are likely to keep happening so long as the testing shortage continues nationwide.

Once a donor is able to secure secondary testing and they’re approved to donate, they then have to make an appointment with a blood bank to have their blood drawn. Sometimes, doing so is no problem. In Orlando, 52-year-old Kevin Rathel recovered after a plasma transfusion from a donor who was screened and approved just 24 hours earlier. Other times, they’re told they have to wait for weeks. In private Facebook groups for COVID survivors, stories of organizations like Red Cross and other blood banks scheduling their appointments for far-off dates abound, with a common sentiment being confusion over why such an urgent donation would take such a long time.
Pranav Reddy, a 29-year-old engineer in Manhattan, says it’s been about 45 days since he reached out to Mount Sinai Hospital and the New York Blood Center to donate, and even though his blood is coursing with the highest concentration of coronavirus antibodies a donor can have, there’s been no word from either organization. The response from blood banks aren’t particularly elucidating. As Red Cross Chief Medical Officer Pampee Young told Today, qualifying patients just “takes a tremendous amount of time and energy.”
Blood banks are the most critical piece of the puzzle when it comes to convalescent COVID plasma therapy, but they face the same uncertainty and pandemic stress that every other business and service is experiencing. According to Louis Katz, a national transfusion expert, former chair of the American Association of Blood Banks and chief medical officer at Mississippi Valley Regional Blood Center in Iowa, furloughs and layoffs have happened at blood banks all over the country, and many locations are reducing their donation hours even if they’re hustling hard behind the scenes to test, prep and store plasma units.
This can contribute to confusingly long wait times for donors, but as Katz explains, it’s also necessary to keep them — and the essential workers at blood banks — safe. It’s the same reason why Katz has instituted extremely stringent requirements on qualifying to donate, requiring documentation of a positive PCR test, rather than merely a “history of COVID” as some centers state. But he also acknowledges that there exists an untapped pool of people who cannot access a PCR test or results, putting in relief how the lack of testing impacts both staff and donor decisions alike.
Given the high number of false positive tests, it’s both a medical and ethical liability to open the floodgates and let everyone who wants to donate plasma in at once, especially considering that social distancing and enforcing low-capacity indoor spaces are, at present, the only known ways to manage the virus’ spread.
“Within my network, on a lot of phone calls, there was a consensus that we probably should wait for 28 days,” he says, referring to how long donors should be symptom-free before they donate. “There are a lot of people that want it done sooner, and I’m getting 50 calls a day saying, ‘You got any plasma? You got any plasma?’ But given that [CPT] is unproven, I don’t think that asking the donors to risk that much is appropriate at this time.”
For donors waiting in the wings, this can be frustrating, to say the least. Neil Holland, a 43-year-old actor and personal trainer in New York City, says he waited for a week to hear back from the blood bank at Mount Sinai after he sent them his initial screening paperwork. Eventually, they called, but he missed it, and despite the four messages he left for them, he had to wait another week for them to get in touch. He was invited back to donate, but when he arrived, he was surprised to discover that they’d only called him in to get an antibody test. More days passed, but when his antibody test came back positive — meaning he was qualified to donate — they never called him back.
Days later, they sent him an email — they were writing to let him know they didn’t need him after all. Apparently, their blood bank was “at capacity for future donors.” “I thought that was really interesting,” he says. “There’s been so much hysteria and panic during this whole COVID situation, and I thought they really needed donors. It was strange to hear there was plenty of plasma.” The whole thing felt like a “discombobulated” communication breakdown to him, and like Kearney, he was disappointed and baffled. “I’m just trying to do the right thing,” he tells us.
Elsewhere, donors are being turned away for equally odd reasons. In Palm Beach, 50-year-old salon manager Rory Posner Corsaw says she was axed from the donor list for “having borne children,” a mistaken disqualification that left her — and other mothers who commented on her Facebook post about it — deeply confused. While it’s true that roughly 20 percent of women do develop an antigen during pregnancy that makes them unable to donate, Corsaw was neither asked whether she had it or given a test to confirm. She was simply told she didn’t qualify and was sent away.
Meanwhile, back in New York City, 36-year-old Lukus Estok says he was disqualified from the New York Blood Center (NYBC) for admitting to a nurse that he was gay. Though he’d been deemed a “perfect candidate” for donation by Mount Sinai and was well beyond the FDA’s controversial requirement that male donors cannot have sex with men for three months before donating, he claims NYBC staffers told him his services weren’t needed and that they’d made a mistake in allowing him an appointment. Even though the FDA had relaxed its restrictions on gay men donating blood and plasma, they “still needed retraining” on how to handle their blood and plasma donations of gay men and told him that updating their system “wasn’t like flipping a light switch.”
In a cell phone video recording shared with us, Estok can be heard pleading with the NYBC manager on duty for an explanation as to why (the manager consented to being recorded). There are no faces in the video, but there don’t need to be — you can tell from the shakiness in Estok’s voice and the way his blue-jean-clad leg trembles violently that he’s hurt and confused, blindsided by the type of treatment he’d thought New York had rid itself of long ago. On the verge of tears, he recounts what happened during his screening to the manager, but all he’s offered in return is an equally shaky description of how the blood center simply hadn’t implemented the FDA’s new rules yet. “I’ve been through a month of hell with this virus,” he says in the video. “I’m finally recovered, I’ve been through a screening process that tells me I’m a potential candidate to donate in a way that might help somebody else, and now I’m being told I can’t.” (Bravo talk show host Andy Cohen had a similar experience.)
“None of it made sense,” Estok says, describing the “intolerable” feeling of being rejected even though he was perfectly qualified. “All any of us really want is to help, to try to save lives during a global health crisis. We need science, not stigma.”
Recently, Wright and the Mayo Clinic have begun to investigate these incidents. Every time they receive a report of an eligible donor being rejected, they call the blood bank where it happened, get the name of the donor who was turned away and attempt to correct the error by inviting them back. What’s more difficult to correct is the cause of that error. As Wright explains, donors are often mistakenly turned away because of “misinformation or some kind of miscommunication that gives the blood bank or hospital employee the wrong idea about the collection process or how badly plasma is actually needed,” he explains. Other times, their investigations have found, the employee who rejects the potential donor is “simply exhausted and doesn’t want to process anyone else.”
In fairness, given that information on coronavirus changes by the day and that many blood banks are working with limited staff and cut hours, mishaps are to be expected. “Every bit of science that has to do with COVID has been accelerated due to urgency and the fact that right now, it’s the biggest threat to mortality we’re facing,” Wright continues. “Normally, there’d be time for preparation before any large-scale study or change to blood bank collections were rolled out to the public, but in this case, because of the direness of the situation, the science and the infrastructure around it is being refined and tested in real time, with most of the hiccups you’d expect from anything that was put together in a hurry.”
In fact, he adds, the entire Mayo Clinic trial was conceived of, designed, approved and rolled out in a little over a week.
So far, Wright says they’ve only received about 10 official reports of mistaken donor rejections, but the actual number of wrongful rejections is probably much higher. None of the people we spoke to were aware that they could have reported their rejection to the Mayo Clinic and most have been able to donate since, so many cases like theirs have likely gone unreported. That said, the Mayo Clinic is working to “open up more channels of communication” so it’s easier for wrongful rejections to be discovered and corrected.
Feeling helpless, physicians themselves are attempting to communicate the urgency of COVID plasma donations to the public. Le even created his own Facebook group to raise awareness for donation and provide some guidance for anyone who might be confused, and so far, it’s inspired a few of them to donate. “It’s just for sharing resources and letting people know there’s a huge shortage,” he explains. “I’m just spreading the word that whoever can help should help. Even if those posts get read by just a few people, I’m hoping it’ll make a difference.”
Again, to be clear, “directed donations” like Kearney did with Boffice early on in the COVID plasma experiment are no longer the norm. And so, while families still plead for donors on social media and attempt to organize testing for them themselves, these kinds of donations have become relatively rare. Instead, the hope in encouraging people to donate is that the more of them who do, the greater diversity of blood types will be available for matching, and the more patients will be able to receive one of the only experimental treatments on the market that might actually help.
What’s Next for Plasma Donors
At the same time that COVID survivors are struggling to navigate the budding plasma donation process for CPT, a second option for donors has emerged: donating not to patients, but for research and development. Over the past few months, a handful of plasma companies like CSL and Grifols have also begun collecting COVID plasma and isolating its vital antibodies to create immunoglobulin treatments and other products, studying how they work but stopping short of doling them out to the sick and dying. Only a handful of plasma companies rule this global market, and the potential for their products to treat successive waves of the pandemic with freshly developed treatments provides a massive opportunity for profit.
Plasma collected via the research pipeline might not lead to the quick results some critically ill COVID patients have experienced with CPT, but there are numerous reasons why potential donors might decide to go that route. For one, nonprofits like the Red Cross don’t pay donors for donations of any kind. CSL, Grifols and other companies do. “The first visit for a donation can take up to two hours and subsequent donations about an hour. Donors are compensated because of this time commitment,” says Grifols corporate affairs director Vlasta Hakes. At all Grifols plasma donor centers, “commitment fees” are put on a prepaid debit card loaded up with anywhere from $30 to $90 per donation, depending on the location. CSL uses the same method, and advertises a monthly haul of up to $400.
As working people struggle to emerge intact from the pandemic, paid donations could be an attractive option for those who have survived the disease, but are still grappling with furloughs, layoffs or economic insecurity. And while the particular donors we spoke to expressed that they were motivated by altruism, not profit, a major portion of the plasma market does rely on people who are drawn to the promise of fast cash.
In fact, in just the past decade, plasma pharmaceuticals have exploded to a more than $11 billion annual market, tripling in growth as both donors and the companies themselves cash in. And that pipeline is only getting bigger: Donation centers in the U.S. have more than doubled in number since 2005, and Grifols alone is investing more than $200 million to build lab infrastructure. So the fact that there is a captive audience of Americans in COVID recovery, ready and looking for cash, is a glaring opportunity for this industry boom to become larger still.
That plasma companies often enforce less strict donation requirements and allow donors to give plasma more often only makes things sweeter. The Red Cross, for example, allows donors to give plasma every 28 days, and in countries like the U.K., you’re only allowed to give twice a month. Plasma companies like CSL, however, allow you to give plasma every two days (though no more than twice a week). Likewise, COVID plasma donors don’t need secondary testing to donate for research. Because their products aren’t being transfused into sick patients, all they need to show proof of is a positive initial coronavirus text and to be symptom-free for 28 days.
Despite concerns that these factors might create a rivalry that only deepens the deficit of available units for the critically ill, Katz is diplomatic when we ask whether plasma companies are essentially competing with blood banks for donors. “The answer is that I don’t know,” he says. “And if that’s the case, I can’t do anything about it.”
This is the reality of doctors and researchers wading into a great, unknown void, taking the unprecedented step to gather a stockpile of COVID plasma that never existed before 2020. His mood on the progress “depends on the day,” Katz jokes; it’s only now, six weeks into the plasma trials, that his blood centers are reporting a stabilized inventory of COVID plasma that’s steadily reaching area hospitals. He remains concerned that donors and hospitals around the country are struggling to keep up, but notes the problems are “entirely dependent and unique to each blood supplier.” Considering that there are 50 independent blood supply hubs around the country, accounting for more than 50 percent of the blood product supply, it’s a machine with a lot of moving parts.
As for Kearney, by the time she was finally able to get to the OneBlood bus and roll up her sleeve, six full days had passed. And though Boffice was transfused with her donation within hours, the red tape and running around meant it had come too late. The next morning, he was dead.
“It was absolutely devastating,” says Kearney. “Crushing. Disappointing. Just horrible.”
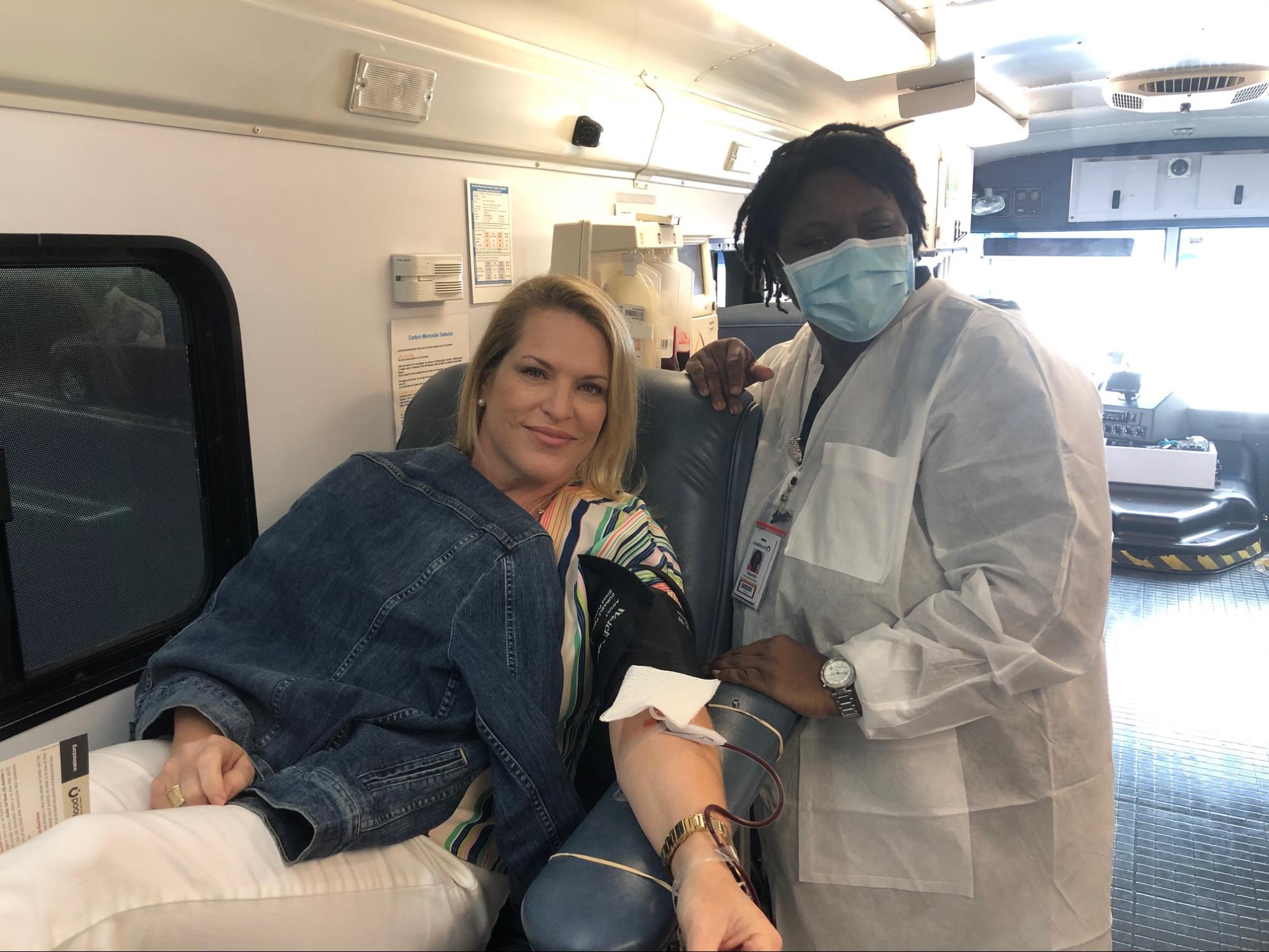
Still, she doesn’t regret a thing. Though her story ended in tragedy, she remains as optimistic as ever about the promise of plasma and is planning on donating again soon. She even hopes to visit Boffice’s family in Canada once it’s safe to travel again. “They said I’m the last person that touched [him], and they want to meet me,” she says. “They consider me family.”
The next time she donates, she hopes things will be easier. In many places, it seems like they already are. Recently, L.A. made virus testing available to “anyone for any reason,” and the Red Cross just began testing convalescent plasma for coronavirus antibodies from pre-qualified donors, to simplify the eligibility process, qualify more potential donors and ultimately collect and distribute more plasma to patients in need. This week, they expect to collect 1,000 units of plasma, a far greater number than the few hundred they rustled up over a three-week period in April. The transfusion rate in the Mayo Clinic study has been improving as well — for reference, Wright reports that on May 4th, 632 of the 702 critically ill patients were transfused, a pattern that’s expected to continue as the national supply comes online.
And while he’s quick to acknowledge that the system hasn’t been perfect so far, he’s also amazed that any of this is happening at all. “The fact that things are functioning as well as they are right now is pretty incredible,” he says. “I’m absolutely floored at how many people have stepped up to help their fellow Americans, most of whom they don’t even know.”
He, like Le, Paneth and nearly every other expert on the CPT case, is every bit as cautious about the future of COVID plasma, but he can’t stress enough how important it is for donors to try to donate anyway. Yes, they might not be eligible; yes, they might have to run around looking for secondary testing depending on where they live; and yes, they might have to wait longer than they want to for an appointment. But if they don’t try, we’ll never know if plasma is really as promising and low-risk a cure as we all hope it is.
“If you have a better suggestion, we’re all ears,” says Kate, the pseudonymous trauma center nurse in the Southeast. “Science is about testing every road thoroughly and proving if something is evidence-based. At this point, so many people are dying that it’s worth it to not just give up.”