“I still don’t really understand what’s going on with the health system, and I’ve been here nearly five years,” says Alistair, a sports journalist who lives and works in New York City. An American citizen by parentage, but brought up in England, he says he’s only now coming to grips with the risky business of insurance. “In Britain you don’t need to understand it — you just go to a doctor and they treat you and then you go home. But here there’s co-pays, deductibles and all these words. It’s just not nice to have that extra stress when you’re ill.”
For someone who had never once had to pay for treatment, nor so much as glance at a medical bill or insurance form until he was in his 30s, Alistair’s experiences in American doctors’ offices have so far made him wary of physicians’ motives. “You’re always suspicious about over-treatment here,” he sighs. When he saw a dermatologist about a worrying mole, for example, it was recommended he undergo a procedure to have it surgically removed. But it wasn’t until afterwards that his friend, a qualified doctor from Australia (which currently holds the dubious title of the worldwide home of melanoma), told him: “That’s bullshit, in Australia they’d have scraped it off. They’ve completely over-treated you there so they could charge you.”
Mike, a content editor in San Francisco — who tells me he’s currently on the hook for $250 from a routine visit to his doctor, which was subsequently contested by his insurers in a way that’s proving far too baffling to challenge — can compare care in the other direction, having lived in the U.K. for two years as a student. Overall, he says he prefers the security and simplicity of Britain’s state-funded, single-payer National Health Service. But he nevertheless sees “occasional perks in the U.S. system, which would mainly be the availability of specialists. I like that it’s pretty easy to shift from a primary care person to a specialist in any situation.” (In the U.K., this isn’t always a straightforward process: Without first getting a referral from a primary care doctor, universally known as a “G.P.” (for general practitioner), it’s usually impossible to see a specialist of any sort.)
And he kind of likes the fact that in the U.S., over-treating and over-referring for minor ailments seems widespread among primary care practices. “In the U.S., they probably err on the side of more tests because there’s a financial incentive for it,” he says. “But I’m okay with that, because I’m a bit of a hypochondriac. So I’d rather get tests for everything, to be 100 percent sure.” Back in the U.K., by contrast, he’d worry that under-treatment was the norm. Often the advice would be, “Take two Nurofen [Advil] and don’t worry about it,” he recalls, “when my dad, who’s a doctor in the U.S. — who obviously doesn’t have a financial incentive — would say, ‘You need to get this checked out.’”
When you next show up at your doctor’s office, then, there are hidden hazards to fall foul of beyond any unexpected charges, whichever side of the Atlantic you’re on. As Mike puts it, “It seems like there are incentives that aren’t necessarily in the patients’ interests in both directions: To save costs in the U.K., and an incentive to spend more in the U.S.”
Without weighing the whole edifice of Britain’s nationally treasured universal healthcare against the U.S.’s more fought-over and fragmented system (although that’s accomplished very nicely here and here — and for a read on how Brits really feel about their NHS, this Twitter feed is always instructive), how primary care is managed in both places reveals a stark divergence in cultures. In the U.S. at least one in three visits to a primary care physician (PCP) results in a referral to a specialist (which is twice as many referrals as G.P.s make in the U.K.) — a trigger-happy trend that’s been on the rise since at least the late 1990s. Jobs in primary care tend to pay substantially less for physicians than those in specialist fields of medicine (it’s the other way around in Britain), and the reluctance of young medics to enter the field is partly why many traditional family doctors’ offices have been shutting up shop across America. According to the Health Care Cost Institute, office visits to PCPs declined by 18 percent between 2012 and 2016, and in April, Walgreens announced it would be launching physician-led primary care clinics at a number of its stores, responding to a desire for more convenient ways to get your check-up.
Against an apparent backdrop of decline in both patient demand and doctor enthusiasm for end-to-end treatment within primary practice, you might wonder why you’re still being shunted through their waiting rooms, when it’s a specialist you really want to see. You might also wonder, since you’re in a diagnosing frame of mind, where all this pressure for referrals and over-treatment is really coming from.
Referential Treatment
According to Daniel Brotman, professor of medicine and director of the Hospitalist Program at Johns Hopkins Hospital, at the level of primary care and in-patient medicine, that pressure isn’t predominantly financial. “Patients often assume incorrectly what those financial drivers are,” he says. “It really frustrates me when I hear accusations that physicians are ordering this, that or the other test — or keeping the patient in the hospital unnecessarily — to make more money. I think financial incentives are increasingly aligned toward less care rather than more care.”
The insurers who approve PCPs to their lists are presumably not fond of paying out for unnecessary procedures, for instance, and neither are employers who pay the premiums, nor the administrators who stump for state-funded care. There’s also increasing awareness on all sides that resources are being stretched throughout the health-care system; in 2017, U.S. health-care spending was at $10,739 per person, more than any other developed nation, accounting for 18 percent of GDP.
Plus, direct financial incentives for gung-ho referrals are heavily restricted by law. Federal “anti-kickback statutes” mean it’s illegal for the doctors themselves to receive any sort of fee for their referrals, nor can they send patients to businesses they have a stake in.
It’s health care, though, so there are gray areas. In December, the Wall Street Journal published an exposé on a trend for hospitals to lean on their in-house physicians to refer internally in order to prevent the “leakage” of business to competitors and instead inspire patient “keepage.” “Hospitals have gained more power over doctors with a wave of acquisitions of practices and hirings in recent years,” the reporters wrote, and “are getting more aggressive in directing how physicians refer for things such as surgeries, specialty care and MRIs.”
And as Sandeep Jauhar, M.D. outlined in a 2009 New York Times article, there are other ways in which physicians might be benefiting from handing off patients to colleagues, perhaps without realizing it. Noting that within professional circles, referring patients can become a form of networking. “When I was in training, simple referrals from internists, like patients with only mild hypertension, bothered me as a waste of time,” Jauhar writes. “Now that I am in practice, I welcome them. [As] a full-fledged doctor, I appreciate the business.” Here, unnecessary treatment might emerge from a culture of professional courtesy, rather than out-and-out grift: “It is hard not to view a referral as an overture from another physician, and it is equally hard not to return the favor.”
Money on the Table
If there are areas where patients might want to keep a wary eye out for truly mendacious medics on the make, says Brotman, it’s much more likely to be a risk in the realm of procedural specialties — surgeries and screenings that carry a premium for their highly trained practitioners. While he believes such abuses of expertise to be uncommon, “that doesn’t mean there isn’t the occasional situation where you might have a greedy doctor who is trying to justify doing extra procedures. If you go to see a surgeon, they make a lot more money being in the operating room than they do seeing you in clinic, and a gastroenterologist is going to make a lot more money in the endoscopy suite.”
Away from these sorts of procedures, though, “when you’re talking about ordering tests and drugs and keeping patients in a hospital for longer periods of time, or admitting them to the hospital in the first place, these are things where there’s really minimal, if any, direct financial incentives for the physician.”
So if it’s largely not to do with harvesting payments, what is driving the health-care industry’s drift toward over-treatment? Together with his colleagues, Brotman has conducted extensive research into the phenomenon in the U.S., and has shown that around a quarter of medical tests, over a tenth of procedures and just over a fifth of medical care overall is unnecessary. He believes the causes for this are diffuse and systemic. Some of the undertow is coming from the patients themselves — from a consumer-culture approach to healthcare (Exhibit A: Walgreens), from a “misperception that more is better,” from “the notion that additional information can’t hurt…” The list, says Brotman, goes on. “We tend to like being offered treatments, procedures and tests, and we need to get away from that.”
Some of the motivation, however, is coming from the other side of the doctor’s desk, where you might have “physicians who are too willing to order things to expedite the care that’s being provided, because they’ve got patients in their waiting room and they need to get on with the next consultation.” Physicians will often be put under pressure from medical administrators too, to ensure the practice is hitting its patient-satisfaction targets — and in any case, says Brotman, in general “we want to please our patients!”
Add both sets of demands together, “and you’ve got a perfect set-up for the physician caving to patients’ requests.” To illustrate, he offers the scenario of someone who turns up at their doctor’s office complaining of a headache and insisting they need a scan. “Certainly it’s not in the primary care doctor’s best interest financially to order a CAT scan. On the other hand, it may be in their interest to do so if they anticipate it’s going to be 15 minutes of counseling that they wouldn’t have time for, if they were to try to talk a patient out of it.”
Acute Subpoena-itis
Brotman is keen to emphasize that the issue of wasteful treatments is due to a whole constellation of factors, and not one thing in particular. Yet another, he notes, is “fear of being sued, because you missed something.”
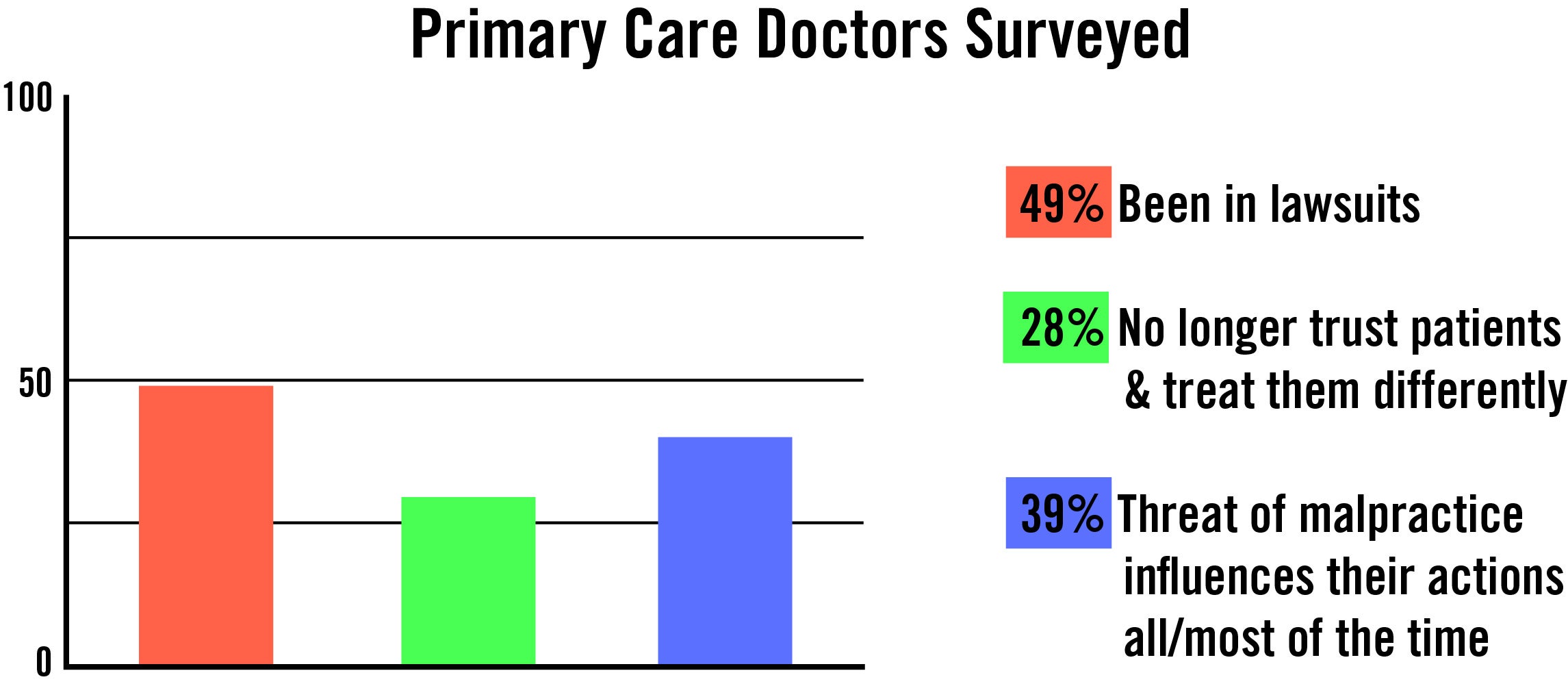
American medicine has a fearsome reputation internationally as a litigation minefield, and according to a Medscape Primary Care Malpractice Report carried out in 2017, which surveyed a total of 4,137 PCPs, this is more than justified. Just under half (49 percent) of the physicians who responded had been named in a lawsuit, and a fifth of those had been implicated for wrongful death. Of the primary care doctors who had been involved in lawsuits, 28 percent said they “no longer trust patients and now treat them differently,” while 39 percent “indicated that the threat of malpractice influences their actions all or most of the time.”
It’s worth noting, though, that it’s not just the American public who have their doctors running for (malpractice) cover. G.P.s in Britain are faring no better — according to a 2017 survey, four out of five reported that concern over being sued had caused them to order needless tests or referrals, while 41 percent admitted to prescribing medication when it wasn’t clinically required.
For an insight into how this trend might be affecting standards in primary care far and wide, Ruth Kannai, a doctor based in Israel, has written candidly of the lasting trauma of a lawsuit brought against her by the family of a man who died suddenly. “It is often noted that doctors practice ‘defensive medicine’ to avert malpractice suits,” she writes. “I know I started down that path after the prosecution. I can’t help being afraid of being sued again. When I reflect on my work since the prosecution, however, I see that defensiveness made me a bad doctor.”
She laments that when a woman walks into her office for the nth time complaining of what she is fairly sure are panic attacks, “the post-prosecution Dr. Kannai cannot allow herself to leave any stone unturned,” and mulls adding to the long list of tests her patient has already had, with “a lumbar puncture, a bone marrow biopsy and an MRI of the brain and cervical spine.” Deep down, though, “she knows that a true family doctor would take the time to encourage, give strength and offer treatment. She would hope for the best. But now, she has joined the cadre of doctors who protect themselves at the cost of their patient’s genuine care.”
Testing Times
Legal anxiety, plus consumer whims, plus physician attrition — it’s a powerful combination of forces all pulling decisive treatment away from the doctor’s offices and into the specialist clinics, operating rooms and hospitals. And it’s leaving a trail of infernally complex billing, contested claims, wasted money and misapplied resources in its wake. Short of remodeling primary care into a rigorous, standardized gatekeeper system in the way that it functions in the U.K., what’s the answer to minimizing waste?
Brotman points to ways we might, “as consumers, reconceptualize what constitutes good medicine.” Is there a way, for example, that we could evaluate orthopedic surgeons based on the percentage of patients they don’t operate on? Because, all things being equal, the best back surgeons would likely be “the ones that operated the least.”
Part of the responsibility for making effective care more efficient lies with clinicians. “We need to think about transparency in monitoring ourselves; we need to have the tools to communicate with patients about why we should be choosing wisely in what we’re doing.” He cites the “Choosing Wisely” campaign, from the ABIM Foundation, as a “wonderful example of a physician-led program to help physicians recognize what they’re doing too much of.”
On a broader scale, he thinks that to address the problem, a whole new perspective is required, from both the public and the health-care industry, which emphasizes medicine as a collective endeavor and not just that individual diagnosis or treatment plan we’re all chasing from one waiting room to the next.
“We all need to recognize that resources aren’t unlimited and the cost of getting care is being borne, even if not by you directly as the patient, by society at large,” he says. “And we need to get in the mindset that in receiving some expensive test or treatment, I’m taking resources for myself that are intended to serve a broad community of people around the country that need medical care. And we have a lot of people who don’t get as much medical care as they truly need. So any time that we’re doing something that costs a lot of money for ourselves, we should be realizing we’re indirectly taking a toll on society.”
As for why it’s probably a good idea for society as a whole to take primary care in particular more seriously, there’s one very good reason that stands out, published this year in a research paper from Stanford and Harvard medical schools. People who live in areas of the U.S. where there is a greater concentration of primary care physicians live longer. On average, the researchers found, for every 10 additional primary care doctors per 100,000 people, a community experiences a 51.5-day rise in life expectancy. So investing more in family doctors and local practitioners nationwide, and supporting them in general wherever you live, would seem to be a wise plan. Because the alternative could leave us all facing the very worst kind of deductibles.

