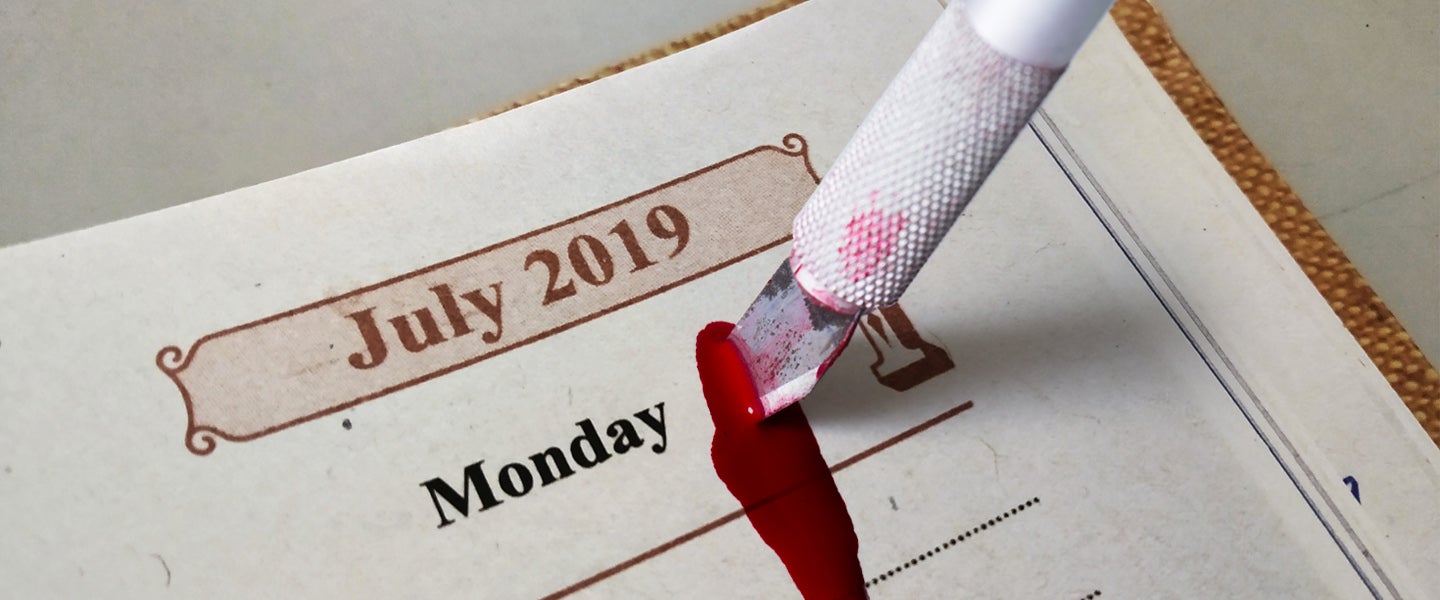
It’s July 1st, 2019, and all across the country, a fresh batch of recently graduated medical students are gearing up for their first day of internships and new residency programs. But as they don their starched white coats and scrub their hands for their first day on the job, many of them ask themselves the same question researchers have been wondering about them for decades: Will I hurt anyone today?
It’s a valid question, given what month it is. July is when thousands of these inexperienced interns and residents are deployed to exam rooms across the country to learn the hands-on skills they need to become licensed doctors. It’s a momentous occasion that honors the passage of knowledge from more experienced hospital staff to fresh-faced newbies eager to learn everything they can, and, as Lisa Schultz, a pseudonymous attending physician who trains new interns at a pediatric hospital in Los Angeles tells me, it’s a “pretty exciting time.”
It’s also a time when these fresh-faced newbies are more likely to mistreat and kill you… or at least it is if you believe in the July Effect. Half urban legend, half demonstrable happening, the July Effect refers to the increase in medical mishaps, medication errors and patient fatalities that can accompany the influx of new interns and less experienced residents into teaching hospitals in July. The same thing happens in August in the U.K., but they have a more colorful name for it: “killing season.”
According to a 2011 meta-analysis published in Annals of Internal Medicine, death rates in teaching hospitals surge between 8 and 34 percent in July, a rate that corresponds to between 1,500 and 2,750 additional fatalities. University of California San Diego researchers also found that fatal medication errors “spike by 10 percent in July and in no other month,” and in Britain, mortality rates rise tend to rise between 6 to 8 percent as new doctors are given tasks they describe as being “beyond their capabilities.” And while the July Effect isn’t well-known enough to be part of most medical school curricula — most doctors I talked to had never heard of it — it does have enough momentum behind it to garner its own dinky saying: “Don’t get sick in July.”
Let me just say if you are ever in the hospital in July confirm everything the "doctor" says with your nurse? #newinterns #scary #julyeffect
— Nora Catherine (@norabell_) July 8, 2014
Paradoxically, other studies have found no evidence of the July Effect whatsoever. Another meta-analysis conducted in 2016 found zero connection between survival outcomes and the month of July, suggesting what many medical professionals like Schultz believe to be true: it might be more farce than fact.
Still, research shows most doctors who have heard of it believe in it, which makes the July Effect somewhat of a medical Bigfoot — some people have seen it and their accounts sound pretty believable, but on the whole, no one’s really sure if it’s real. Over 200 studies have been conducted on the phenomenon in the past few years, and while there seems to be evidence for it, most research has come to the following conclusion: “No one fucking knows.” It’s been observed in some hospitals in some studies, but beyond that, the medical community can’t seem to agree whether the July Effect is an actual thing, or just a media-inflated myth inspired by a few horror stories that give the whole month a bad name.
I, however, am not satisfied with such flippancy. What if I get sick in July? What if I fall and fracture my spleen? I need to know whether it’s safe to go buck wild this month and run my jet ski into an amoeba-infested pond or if it’s better to cower inside with hand sanitizer and a helmet to avoid any potential hospital visits. But because the research is conflicting, I knew I needed to go straight to the source to try to find out whether this year’s crop of hot new hospital interns were really as green and murderous as the scary internet made them seem.
Figuring there was no one better to ask than one of the eager beavers themselves, I called my friend Jared Brenner (also a pseudonym), who, as luck would have it, starts his internship at a teaching hospital in Temecula, California, today. In fact, he’s probably there right now.
Brenner is in internal medicine, a catch-all field for what he describes as “hurty organs.” As he progresses through his multi-year internship and subsequent residency, he’ll eventually specialize in pulmonary critical care, but for now, he’ll be doing miscellaneous, basic doctor stuff: making diagnoses, writing prescriptions and doing his best to uphold the Hippocratic oath: “Do no harm.”
When I ask if he feels medical school has adequately prepared him to hold life and death in his hands this July (or at the very least, someone’s colostomy bag), he gives me a staunch affirmative. “I feel good about it,” he says. “This isn’t going to be the first time I’ve seen a patient and had to make decisions about their care.”
New interns don’t enter the exam room anywhere near as fumbling and unprepared as the July Effect makes them seem, he explains. They’ve just come from medical school, the last two years of which are spent getting their clinical hours in, speaking to and examining patients under the guidance of professors and practicing physicians. “You see many, many patients before you ever start your internship,” he says. “The only difference is that in medical school, the doctors are making the real decisions. Once you hit your internship though, it’s all you.”
Er, sort of — though July marks the time when interns can start diagnosing and treating patients on their own, Schultz tells me they can barely budge without having to report to an attending physician, a resident supervisor or a seasoned, all-knowing nurse first. “There’s not a single thing you do during your internship or residency that a more experienced person doesn’t have to sign off on,” she says. “There’s a safety net for everything. With all the oversight and levels of approval, and the increased level of vigilance in July, it’s actually kind of hard to slip up and hurt somebody.”
Yet, slip up they do.
In 2012, oncology nurse Teresa Brown wrote an op-ed in the New York Times called “Don’t Get Sick in July” in which she tells the story of a time she had to go outside the all-important chain of command in order to give a cancer patient who was suffering in agonizing pain a morphine pump. This, she writes, is something the first-year resident on call had patently refused to do. “The resident might have learned in medical school about pain during dying, but he had not actually been with a patient going through it,” she writes. “Seeing such pain — the body twisting, the patient crying out helplessly — is categorically different from reading about it.” Had she not paged the palliative nurse on call who immediately agreed that the man needed morphine yesterday, he would have continued to suffer until his final moments, which came not long thereafter.
Reddit’s got a couple horror stories of its own as well. Writing in a r/todayilearned thread about the July Effect, redditor lackofcommitme says he once had a new doctor practice setting a bone when he broke his hand. “I had fractured the knuckle of my ring finger,” he says. “Two hours of unsuccessful attempts later I had a spiral fracture in my pinky and a second fracture on my ring finger’s metacarpal that required surgery.”
My own stepfather even had a little July Effect mishap of his own last year, which is actually how I found out about it in the first place. Though he’d fallen off a roof and shattered his ankle (he’s fine), an intern had mistaken his chart for the chart of someone who was recovering from a heart attack. So, for three full days, his very broken ankle went ignored while he received treatment for his heart instead (which there was nothing wrong with.) He was on too many drugs to realize what was happening, my mother and I weren’t medically literate enough to pick up on the nuances of what they were doing and it wasn’t until his regular doctor returned from a long weekend that anyone realized the error. I was there when the physician muttered something like “fucking July” under his breath.
From what Brenner knows about the July Effect (and what most research seems to show) incidents like these are extremely rare. But, when they do happen, it’s usually because of one of two things. The first is overconfident interns and residents. “If you have a ‘can’t tell me nothing’ attitude and walk around like you already know everything, you’re probably going to wind up hurting somebody,” he says. However, he’s never met anyone like that personally, and has only heard about it happening elsewhere once or twice. Mostly, he says, interns are cautious, receptive, humble and eager to learn and care for their patients.
The second factor that makes newbies more likely to hurt their patients are senior residents and attending physicians who give their interns a little too much freedom. Once, when Brenner was still in medical school, a surgeon who was supervising him asked him to remove a central line (a catheter that feeds directly into the heart from one of the body’s largest veins) from one of her patients, then promptly disappeared to lunch, leaving him on his own.
Though he’d done it once before under direct supervision, he didn’t feel anywhere near prepared enough to do it without supervision, so he asked one of the nurses on call to show him the ropes. “It was a little iffy of her,” he says. “That was one of those super rare situations when the safety oversight wasn’t exactly there.” But, that was in medical school. Brenner says he doesn’t expect anything like that to happen during his internship. And if it does? Well, he says, that is how you learn.
“Regardless of whether or not you believe in the July Effect, you can’t avoid the fact that in medicine, you have to learn by doing,” he says. “You don’t become a good doctor by taking notes and nodding. There will always be situations in which a less experienced person has to do something they’re unfamiliar with, which means there’s always the potential for higher risk if they’re not being supervised properly.”
Thankfully, says Schultz, hospitals are very aware of this risk. “July is definitely a tenuous time,” she says. “We treat it differently than any other month because we know how green the interns and new residents are. They absolutely need more supervision than they do in later months.” When I ask her if she thinks that means the July Effect is real, she doesn’t hesitate to respond that she does…but with a big caveat.
“I can definitely confirm that people make more mistakes than almost any other time,” she says. “People write incorrect orders, give the wrong dosage and forget crucial information. Thing is, these mistakes are almost always caught.” For example, if one of her interns writes a prescription for a dose of oxycontin that’s far too high, it’ll get reviewed by a senior resident, an attending physician and the pharmacist on-call before it ever gets anywhere near the patient. Many programs have also enacted other July Effect-combatting changes to minimize the risks newbies pose, such as electronic records training and education on patient handoffs and the discharge process. Schultz also says there’s almost always a pharmacist on call in teaching hospitals to help minimize medication errors as well.
Even more telling, however, is the fact that July isn’t even the worst month to go to the hospital. It actually has better medical outcomes than January and the time period around the holidays. So, if you must get sick or break your femur, the hospital is actually relatively safer in July, even with the July Effect taken into account.
That’s why Schultz says the July Effect is probably real, but vastly overblown in terms of what it means for both interns and patients. When her mother broke her hip last July, she was treated by a flock of new interns and residents who didn’t seem to be entirely sure what they were doing, but still, she trusted that her mom was in good hands. “Having gone through the same process myself, I knew nothing they were doing wasn’t being supervised,” she says. “I felt completely confident that they’d take good care of her. I’d say the same thing if my own child needed to go to the hospital in July. I’d feel just as calm. Just because some people aren’t as experienced doesn’t necessarily mean you’ll get worse care.” Surprise, surprise: Her mom was fine.
#JulyEffect My brand new intern has already written down key learning points from rounds in the little notebooks we provide, one hour into his first rotation. Learning can coexist with safety; we're all going to be just fine. #TheKidsAreAlright
— Sharmila Dissanaike (@DissanaikeMD) July 2, 2018
She also cautions against thinking you shouldn’t go to the hospital in July if you need help. “It is always better to go to the hospital if you need to than it is to buy into the legend of the July Effect,” she says. “Medical errors are rare, but it’s important to not that they happen at all times of the year, in all types of facilities, not just teaching hospitals in July. It’s not like everything’s fine until June 30th and then everyone starts dying on July 1st.”
What that means for your weekend is this: even if the July Effect is real, a lot more research is needed to understand how it works. In the meantime, it’s probably not going to affect you in any appreciable way. Amoeba pond, here I come.